Insights from a Health Talk FM.102 Interview: Headaches - Assessing the Risks
Insights from a Health Talk FM.102 Interview: Headaches - Assessing the Risks
How dangerous are headaches?
The most prevalent complaint among patients admitted to the neurology department is headache, a symptom commonly associated with the nervous system. This condition can be attributed to the changes in modern society, where individuals are constantly in a rush, experiencing high levels of stress and sleep deprivation. However, it is important to note that headaches are not solely caused by stress or lack of sleep; they can also serve as a significant indicator of potentially severe ailments that may result in disability or even death.
Headaches can manifest at any age, with a higher incidence observed among individuals in the working-age bracket, as well as middle-aged and elderly populations. Each age group possesses varying susceptibility to different diseases. For instance, working-age individuals may be prone to less perilous conditions, while older adults are more likely to encounter more severe ailments. To simplify the categorization of headache symptoms, patients can be divided into two distinct groups: those exhibiting dangerous symptoms and those displaying non-dangerous symptoms.
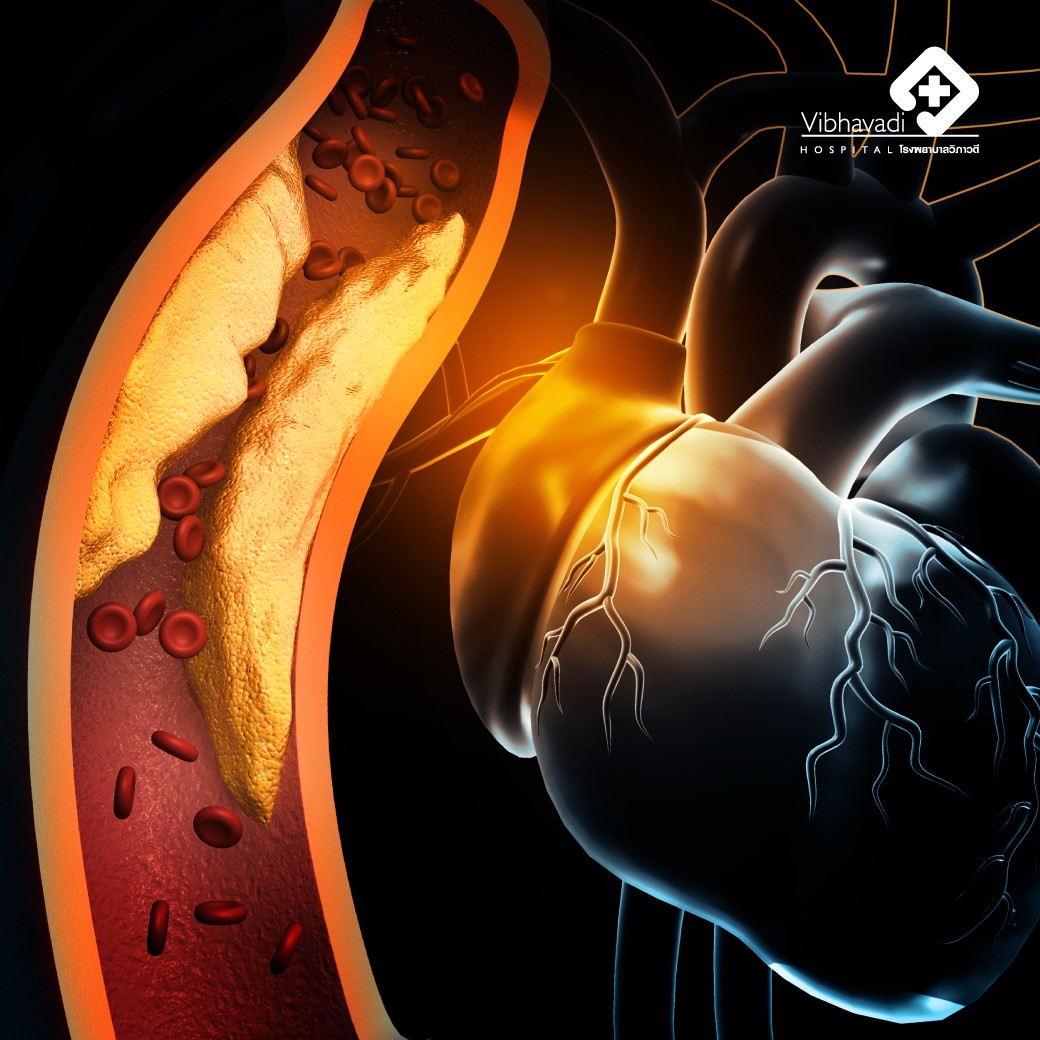
In the category of non-threatening headaches, we commonly encounter conditions such as migraines and tension headaches (also known as headaches caused by muscle spasms or tension in the muscles). These types of headaches can be characterized as muscle tightness. Another example is cluster headaches, which may sound familiar to some. However, there are more types of non-dangerous headaches apart from these, while the dangerous group includes conditions like brain tumors, brain hemorrhage, ischemic stroke, meningitis, and occasionally shingles affecting the nerves in the brain.
In the case of non-dangerous headache conditions, such as migraines, they often exhibit distinct patterns. Generally, these headaches come and go, with a period of complete recovery in between. The duration of each specific condition varies; for instance, migraines should not last more than 3 days, while tension headaches may persist for days or weeks, depending on the triggers. Cluster headaches, on the other hand, occur for no longer than 3 hours at a time, but they can appear 2-3 times within a day, forming a series known as Cluster Migraine. The pain is typically concentrated on one side, although it can occasionally affect the other side, alternating between the right and left. Throbbing pain and significant discomfort are common characteristics, often accompanied by symptoms like nausea, vomiting, and a preference for remaining still in a quiet, dark place due to sensitivity to light, sound, and vibrations. Heat or warm temperatures can act as triggers for some individuals. Tension headaches are primarily caused by stress and sleep deprivation, and they create a sensation of pressure around the head, leading to persistent pain throughout the day. They frequently occur during working hours. Cluster headaches, however, persist on one side for an individual's lifetime. For instance, if the pain was previously experienced on the left side, it will continue to affect the left side. The pain is typically focused around the eye socket. Notably, autonomic nervous system symptoms accompany cluster headaches, such as swelling of the eyelid on the affected side, nasal congestion, and tears flowing from the same side. These symptoms disappear once the headache subsides and should not last longer than 3 hours.
The treatment approach varies depending on the type of headache. For migraines, there are specific medications available, such as triptans or ergots (although ergot usage is rare due to its side effects of excessive blood vessel constriction throughout the body). Instead, general painkillers and anti-migraine drugs are commonly used. In cases where the patient experiences frequent pain, occurring more than 2-3 times a month, continuous study and observation of the symptoms are crucial. Identifying triggers plays a significant role, and it is advisable to study and avoid these triggers.
In the case of migraines, if the pain begins, taking paracetamol can be helpful. Prompt medication intake during the aura phase (if the patient experiences aura before the onset of the headache) can lead to quick relief. Aura symptoms may include blurred vision, dizziness, and visual disturbances. For tension headaches, the focus is on reducing trigger factors, such as stress, ensuring sufficient sleep, and regular exercise. Painkillers are effective in managing the pain, and in some cases, antidepressants can also be beneficial. It is important to note that most painkillers for tension headaches are nonsteroidal anti-inflammatory drugs (NSAIDs), which can have stomach-related side effects. Therefore, if not necessary, they should not be taken for more than 5 days. If absolutely required, the maximum frequency should not exceed 15 days per month. Cluster headaches are less common but can be more intense. Oxygen therapy has shown positive results in alleviating cluster headache pain. However, it may not always be convenient for patients to always have access to oxygen, especially at home. In such cases, medications similar to those used for migraines can be employed, along with a preventive medication specific to cluster headaches. The administration of oxygen typically lasts for about 15 minutes to provide relief.
The dangerous groups of headaches can be identified through the following observations:
1. Rapid and intense onset: If the headache escalates from no pain to severe pain within a short period, such as within 1 minute, it is considered dangerous. This sudden and intense progression may indicate conditions like bleeding in the brain.
2. Late-onset headaches: Individuals who have never experienced headaches before, but suddenly develop pain after the age of 50, are at higher risk. Most non-dangerous headache conditions, such as migraines, tension headaches, or cluster headaches, typically manifest before the age of 50.
3. Altered patterns: Individuals who have had recurring headaches with a specific pattern, but suddenly experience changes in intensity, location, duration, or pain characteristics, should be cautious. These alterations, such as increased violence of the headache, shifts in pain location, longer duration, or awakening from sleep due to pain, are worrisome signs.
4. Neurological symptoms: The presence of additional neurological symptoms alongside the headache, such as sudden weakness, double vision, ringing in the ears (tinnitus), slurred speech, unsteady gait, or a stiff neck, should raise concerns about potential danger.
5. Underlying congenital diseases: Individuals with certain congenital conditions, especially those associated with low immunity, should be particularly cautious. For example, individuals with systemic lupus erythematosus (SLE) who are taking immune-suppressing medications should be suspicious of a potentially dangerous headache, as it could indicate an infection-related complication. These cases require closer attention due to the increased vulnerability. These observations help identify dangerous headache groups, which can include various conditions ranging from brain tumors to cerebrovascular diseases and meningitis. If the pain prevents sleep, it is particularly concerning, as sleep is typically considered a protective factor in non-dangerous headache conditions, often providing relief.
The location of pain plays a significant role in assessing the nature and progression of a disease. When seeking medical attention, doctors often inquire about the location of pain and its characteristics to aid in diagnosis. Specific pain locations can provide valuable information. For instance, pain concentrated in the eye sockets may indicate conditions like glaucoma, cluster headaches, or migraines. Patients should also take note of pain in other areas such as the forehead, temples, occiput (back of the head), or the middle of the head, as these positions can help the doctor make a more accurate diagnosis. Some diseases may cause pain throughout the entire head or in specific regions. However, patients' observations and descriptions can significantly assist in the diagnostic process. If there are signs of potential danger, such as worrisome symptoms or indications, a brain scan will likely be conducted to confirm any abnormalities in the brain. In cases where symptoms resemble meningitis, such as fever, generalized headache, nausea, vomiting, and a stiff neck, a lumbar puncture may be necessary to collect cerebrospinal fluid for further analysis. In certain situations, where there is suspicion of cerebral masses or cerebral ischemia, a detailed brain scan like an MRI (Magnetic Resonance Imaging) may be preferred, as it offers more comprehensive visualization. An MRI can include MRA (Magnetic Resonance Angiography) to assess the arteries or MRV (Magnetic Resonance Venography) to evaluate venous constriction that can cause headaches. Conversely, if there is a suspicion of bleeding, a brain CT scan may be performed, potentially accompanied by MRA or MRV to provide additional information.
The nature of the disease can be classified into three basic types based on the description of the pain:
1. Throbbing: A pulsating sensation synchronized with the heartbeat, indicating possible conditions related to vascular issues or migraines.
2. Sharp: A distinct, acute, and piercing pain, which may be associated with peripheral neuropathy.
3. Squeezing or tightness: A sensation of pressure or constriction, as if something is pressing on the head. This type of pain can be attributed to various causes, ranging from normal muscle tension to more serious conditions such as brain tumors.
The duration of the disease is an important factor to consider. Most benign conditions follow a pattern of recurring episodes with periods of complete recovery. The duration of each disease varies. For example, migraines typically last no more than 3 days at a time, with pain resolving before a new episode begins. Cluster headaches usually do not exceed 3 hours per episode, but multiple episodes can occur in a single day. Tension headaches may persist for days or weeks before subsiding. In contrast, the most dangerous diseases often have pain that does not go away completely, even with the use of pain medication like paracetamol. Symptoms associated with tumors may gradually worsen over time, while bleeding-related pain may have distinct characteristics, such as rapid onset and intensity that may stabilize but not fully disappear after taking pain medication. Noting what triggers or alleviates the pain can also aid in diagnosis. Patients should pay attention to activities or circumstances that improve or worsen their symptoms. For example, resting or getting adequate sleep may alleviate migraines for some individuals, while others may experience relief after vomiting, which often signals the end of a migraine episode. Therefore, these observations can provide valuable insights into the likely diagnosis.
Additionally, ensuring a good night's sleep is crucial, with at least 7 hours of uninterrupted sleep and high-quality sleep without disturbances. Poor sleep quality, such as snoring, can contribute to more frequent migraines. Patients should also be mindful of activities that worsen their symptoms, such as coughing, sneezing, or straining, as these may suggest increased intracranial pressure. Joint symptoms are important to consider as well. If fever, stiff neck, and generalized headaches are present, meningitis may be suspected.
The occipital area, located at the back of the head, can be associated with various diseases and conditions causing pain. Migraines, for example, can sometimes manifest as pain in the back of the head. Tension in the muscles of the neck can result in neck pain that radiates to the occipital region. Occipital pain can also be attributed to degenerative cervical spondylosis or even brain tumors. Apart from considering the location of the pain, other common symptoms and the nature of the disease are taken into account during the diagnostic process. Observing how the pain responds to certain actions or positions and assessing overall bodily symptoms are also important factors.
When seeking relief for muscle or cervical pain, it is crucial to exercise caution when receiving massages. Massages, particularly those involving stretching techniques, can be beneficial and provide relief. However, it is essential to ensure that the massage techniques used are correct. Improper methods, such as excessive twisting of the neck, can lead to blood vessel tears, which can be dangerous.
Certain benign headaches, like migraines, may improve as we age, potentially due to lifestyle changes. However, most of these headaches tend to persist in our lives. They can reoccur when triggered by certain factors. For instance, migraines may be triggered by consuming certain foods like coffee, alcohol, cheese, foods with high MSG content, or nitrates found in Chinese sausages. Lack of sleep or living in excessively hot weather can also act as triggers. It is crucial to be mindful of these triggers and make necessary lifestyle adjustments. When the pain occurs, specific pain medications may be required. Taking the medication promptly when sensing the onset of a migraine can help alleviate symptoms quickly and reduce the need for excessive painkillers. Monitoring the frequency of migraines is important. If they occur too often, preventive or control medications may be necessary. These medications aim to reduce the frequency and intensity of migraines, making them more manageable.
Some individuals may prefer non-medication approaches. For instance, for tension headaches or tight muscles, physical activities and stretching exercises can be beneficial. Engaging in physical stretching routines not only helps with muscle relaxation but also alleviates these types of headaches.
In terms of self-care, it is essential to pay attention to the characteristics of our headaches to determine whether they are indicative of a more serious condition. Seeking prompt treatment can increase the chances of healing and prevent potential complications associated with brain diseases.
Pongsakorn Tanayapong, M.D., Neurology Physician